01. Overview And Background
Concept rendering from the master plan of a future vision for the Austin State Hospital Campus, reimagined as more than a hospital, but a platform for the entire continuum of care for a brain health system. Image created by Page/ for Dell Medical School.
Mental disorders, including substance use disorders (SUD), are perhaps the most misunderstood and stigmatized medical conditions affecting humankind. These conditions are now widely recognized as brain-based illnesses. Through our qualitative research, we learned that the term “brain health” does not hold the same stigma that “mental health” does, and the commonly used term “behavioral health” is misleading and poorly understood by the public. “Brain health” appropriately expresses these illnesses as the medical conditions they are, rather than just sets of behaviors that are often misunderstood. However, since the term “mental health” is more commonly used, in this document, we interchangeably use both “brain” and “mental” health to continue to advance toward less stigmatizing terminology.
With these considerations in mind, Texans deserve the best brain health care available, regardless of an individual’s specific socioeconomic resources. To achieve this vision, investments in our public mental health care must be thoughtfully leveraged to optimize outcomes. Texas is investing in its public and private brain health institutions and treatment programs to anchor the research, training and service delivery necessary to meet this goal. This report is part of that investment, focused on mental health care delivery in the Austin State Hospital (ASH) Service Area.
The Texas public psychiatric hospital system is facing multiple issues including wait lists, increasing forensic (justice-involved) demand, aging facilities, operating inefficiencies, staff turnover and hiring challenges. Despite efforts to close service gaps, the delivery of brain health care remains fragmented; at a structural level, it continues to relegate our state’s most pressing mental health needs to an outdated system that separates brain health from the rest of medical care, and individuals from their communities. Texas excessively relies on jails, emergency departments, crisis management, and outdated state hospitals to deliver brain health care. The intersection between the mental health and legal systems is fraught with inefficiencies, delays, unnecessary expenses and suboptimal outcomes, inadequately serving both individuals seeking care and the court systems. However, with the current investments, evidence-based models, and deliberate and informed planning, Texas can become a national leader in public brain health care, as it is in many other areas.
“…we interchangeably use both ‘brain’ and ‘mental’ health to continue to advance toward less stigmatizing terminology.”
One defining step toward this vision occurred in 2013 when the Department of State Health Services (DSHS), which operated the state hospitals at that time, requisitioned a 10-year study by CannonDesign (“the Cannon Report”) of the state psychiatric service infrastructure. This report supported observations in the previous paragraph and made a number of recommendations based on a goal to provide Texans the right care at the right place at the right time. One recommendation was the need to replace several state hospitals that have fallen into such disrepair that total replacement is more cost-effective than renovation and is necessary to develop facilities specifically designed for modern-day care. The Cannon Report estimated the inpatient capacity to capture unmet needs, system backlogs and expected population growth. The 85thTexas Legislature responded robustly to this report by appropriating significant funds, leading to construction projects planned or underway in Rusk, Houston, Austin, Kerrville and San Antonio. The Cannon Report also highlighted a number of equally if not more important system changes that could impact the design of state inpatient facilities and improve access to and quality of mental health care. Several of these recommendations are specifically relevant to needs in Central Texas that will be addressed in this report including:
In addition to building public inpatient facilities, the Cannon Report proposed better use of private psychiatric hospitals closer to where people needing services live. It suggested shifting short-term acute inpatient care to Local Mental Health Authorities (LMHAs) and community and private psychiatric hospitals. Health and Human Services Commission (HHSC) adopted this approach but expansion is needed to allow state hospitals to focus on providing long-term subacute and residential care for persons with complex needs that cannot be obtained elsewhere.
The Cannon Report emphasized expanding use of alternatives to hospitalization whenever clinically possible to improve clinical outcomes, decrease costs, improve hospital throughput and hence increase inpatient capacity.
The Cannon Report recommended building an infrastructure integrated into existing and expanded community ambulatory and inpatient medical and substance abuse resources, include Federally Qualified Health Centers (FQHCs), LMHAs, and other health care facilities. This approach emphasizes embedding brain health back into the general delivery of medical care, as discussed in the opening paragraph of this report.
The Cannon Report recommended improving the structure of forensic pathways to reduce waitlists for mental health care within the criminal justice system and decrease time to initiating treatment. Opportunities to build on recent Texas statutory changes permitting alternatives to inpatient competency restoration open the door for these improvements.
The Cannon Report recognized that the designs of existing state hospitals impede efforts to support modern mental health care recommendations and delivery. New hospitals must incorporate advances in psychiatric hospital design (e.g., single occupancy rooms) to enhance care.
Finally, the Cannon Report emphasized the need to increase workforce development, to build both quantity and quality of professionals providing mental health care.
The full Cannon Report is provided as Appendix 1. Importantly, these recommendations require HHSC to expand meaningful partnerships with private, public and academic entities. These considerations are central to many of our recommendations. Our proposal, then used the Cannon Report both as a starting point and to contextualize our recommendations.
In parallel with work leading to the Cannon Report, the Texas Legislature created within HHSC the position of Associate Commissioner for Mental Health Coordination, which led to development of a Behavioral Heath Strategic Plan (“Strategic Plan”) to initiate mental health care transformation. Consistent with Cannon Report recommendations, the Strategic Plan set a vision “to ensure that Texas has a unified approach to the delivery of behavioral health services that allows all Texans to have access to care at the right time and place.” The Strategic Plan set a goal to create measurable improvements in coordination across different mental health and substance use disorder agencies. This goal of the Strategic Plan aims to improve awareness of and access to mental health and substance use disorder services, so that people suffering from these conditions are less likely to become involved in the criminal justice system, die from comorbid conditions earlier than the general population, or require, especially extended, inpatient psychiatric hospitalizations. To achieve this vision, the Strategic Plan proposed short and long-term approaches to fill a number of gaps in the current mental health care continuum, several of which are particularly relevant to redesigning the care within the ASH Service Area, including:
improving access to the least restrictive, evidence-based mental health services, including substance use disorder services;
improving access to timely mental health and substance use disorder treatment (including to individuals waiting in jails);
expanding access to supportive housing; and
decreasing shortages within the mental health workforce.
The entire Strategic Plan, and a recent update, can be found online (BHSP) (BHSPupdate). Again, this current report used the Strategic Plan to frame our recommendations.
In response to these needs, the 85th Texas legislature invested significantly to advance the mental health care of its citizens. This current ASH project specifically arose from a $300M investment described in Budget (SB1) Rider 147 “for the planning of new construction projects at the state hospitals and other state-funded inpatient mental health facilities in current and future biennia.” Specifically, Rider 147 requested from HHSC a “comprehensive inpatient mental health plan for the replacement or significant repair of state hospitals or other state-funded inpatient mental health facilities to expand inpatient mental health capacity over the next three biennia” (HHSC’s “A Comprehensive Plan for State-Funded Inpatient Mental Health Services” is provided in Appendix 2). Additional legislative intent toward implementing hospital redesign is described in Riders 145 and 147; specifically, the Legislature encouraged academic/public partnerships with HHSC in order to “develop a master plan for the design of neuropsychiatric health care delivery systems in the area served by each facility” (riders are included in Appendix 3). This specific charge previously arose from a DSHS special report in September of 2016 that emphasized the value of leveraging the expertise of academia toward improving mental health care in Texas universities (AcademicPartnerships). When possible, the development of this recommendation, which includes a master plan was to “be led by the public or private entity with which HHSC has partnered.” With these Legislative mandates in mind, HHSC approached Dell Medical School (DMS) of the University of Texas at Austin to lead the redesign of the Austin State Hospital (ASH) and the delivery of mental health services in the ASH Service Area. Dell Medical School was the natural partner for this project given its location in Austin and its commitment to improve community health. Together, then, DMS and HHSC partnered to tackle this important task with $15.5M to complete preplanning and construction planning phases of this project.
“…a new facility is a critical and necessary first step, this step alone will not produce the optimal mental health care system for the people of the ASH Service Area.”
As we describe in this report, the ASH campus is the right place to begin the integration necessary to realize the Texas vision of a revitalized, optimally funded high-quality mental health care system. As identified in the Cannon Report and prioritized in HHSC’s Comprehensive Plan, the ASH facility is sorely in need of replacement, providing a unique opportunity to change how psychiatric care is delivered throughout the ASH Service Area. Moreover, this Service Area includes collaborative regional leadership among LMHA, hospital districts and other safety-net hospitals, legislative leaders, community business and philanthropic leaders, HHSC, and the new Dell Medical School. Consequently, in this document we propose the initiation of the ASH Brain Health System Redesign that would establish a continuum of inpatient and outpatient brain health services anchored on the ASH campus to drive improvements in full partnership with existing mental health and substance use disorder treatment systems throughout Central Texas. We provide specific plans to replace outmoded ASH buildings with a modern inpatient facility and operationalize the broader redesign of the care continuum within this Service Area. Importantly, we emphasize that although replacing ASH with a new facility is a critical and necessary first step, this step alone will not produce the optimal mental health care system for the people of the ASH Service Area. Therefore, additional recommendations are provided that identify a broader approach toward this important goal as an integral part of the mission of the Texas Statewide Behavioral Health Strategic Plan. The remainder of this report describes these recommendations.
Key Points – Overview and Background
• Austin State Hospital has aged past the point of restoration and must be replaced.• This replacement provides a unique opportunity to evaluate and improve mental health service delivery across the ASH Service Area.
• The proposed plan builds from prior investments and work by the state.
• Dell Medical School contracted with HHSC to convene these planning processes.
Approach
Prior to the 85th Texas Legislative Session, a number of key stakeholders in Austin were actively collaborating toward improving the mental health care system in Travis County. With the support of the legislature, from this core group we quickly organized a working team for the Preplanning Components of the ASH Service Area redesign (i.e., this report) in order to meet the legislative goals previously discussed. Specifically, we established a Steering Committee to drive the Preplanning Process, comprised of regional stakeholders and led by Dell Medical School’s Associate Vice President, Regional Mental Health (Steve Strakowski, M.D.). The membership of the Steering Committee is provided in Table 1 and detailed in the initial Steering Committee Charter (Appendix 4). Please note that changes in personnel occurred after the initial charter was signed to accommodate new considerations with the planning process.
● Health Institution: Committee Chair - Steve Strakowski, M.D., Associate Vice President, Dell Medical School (DMS)
● Health & Human Services Commission: Tim Bray, MA, JD, Associate Commissioner, State Hospitals
● Local Mental Health Authority: David Evans, CEO Integral Care (Travis), Andrea Richardson, Executive Director Bluebonnet Trails (Bastrop, Burnet, Caldwell, Fayette, Gonzales, Guadalupe, Lee and Williamson)
● Healthcare District: Mike Geeslin, CEO Central Health (Travis)
● University of Texas System: David Lakey, M.D., Vice Chancellor for Health Affairs
● Texas Hospital Association: Sara González, Vice President of Advocacy/Public Policy
● Texas Organization of Rural & Community Hospitals: Scott Briner, CEO, Sweeny Community Hospital Development (Brazoria)
● Law Enforcement: Sheriff Dennis Wilson (Limestone)
● Peer/Family Representative: Karen Ranus, Executive Director, NAMI Austin (Travis), Jason Johnson (Kerr)
● Internal Design Consultant: Beto López, Managing Director, Design Institute for Health (DMS)
● Ex Officio: Jim Baker M.D., MBA (DMS), Sandy Hentges Guzman (Office of Senator Kirk Watson), Octavio Martinez M.D. (Hogg Foundation), Lisa Owens (Central Health), Katherine Jones (DMS), C. Martin Harris, M.D., MBA (DMS)
One of the first actions of the Steering Committee was to develop a list of core principles to drive the Preplanning and Planning processes. These principles are:
Taking excellent care of people is always the first priority in planning with a goal to provide the right care at the right time in the right place.
The best evidence-based models for care are embedded in the design.
The ASH Campus will serve as a platform for brain health care innovation and delivery across the Service Area.
Collaboration among academic, public and private partners will be central to the design.
The redesign will eliminate over-reliance on jails, hospitals and emergency departments.
Programs and facilities will be designed in which cost reflects the right level of care.
The design will improve operational efficiencies in the ASH Service Area.
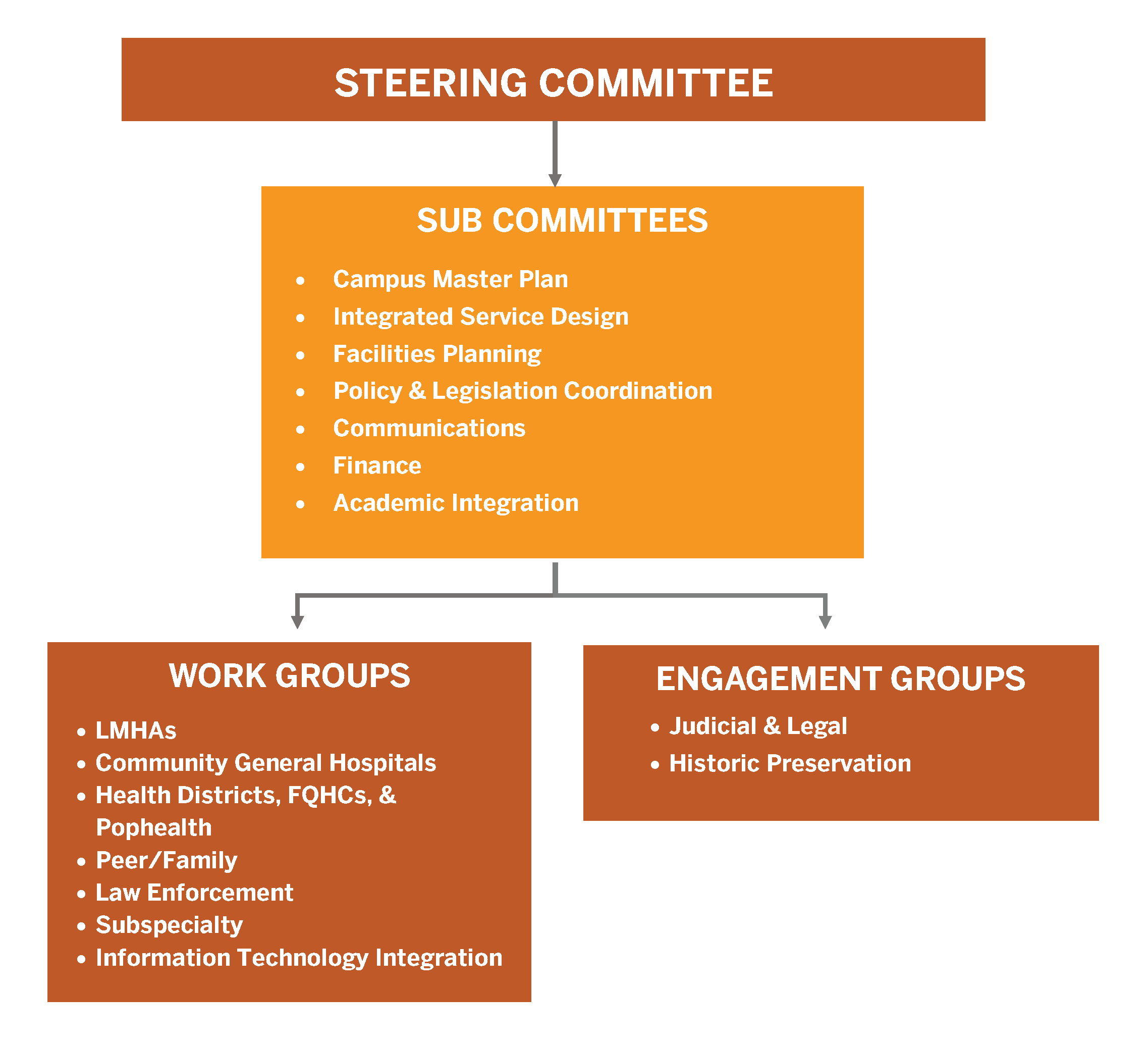
Throughout the process, the Steering Committee committed to collaboration, transparency, inclusivity and engagement across as much of the Service Area and as many stakeholders as possible. To accomplish this commitment, a planning cascade was created that extended from the Steering Committee as illustrated in Figure 1. A complete list of all of the participants in these various subcommittees and workgroups, as well as a number of other individuals, who were consulted formally or informally, provided in Appendix 5.
Upon release of funding from the Legislative Budget Board (LBB) and Governor Greg Abbott to HHSC, the Preplanning contract between HHSC and DMS was completed effective February 1, 2018. Preplanning Staff were hired and the formal work was initiated. Following the procurement processes of the University of Texas, the Meadows Mental Health Policy Institute (MMHPI) was subcontracted on March 21, 2018 to provide critical data gathering and analytic resources and Page Southerland Page, Inc. (Page/) on June 18, 2018 to create the ASH campus Master Plan (Appendix 6). Specific components and processes followed during Preplanning are outlined in a Gantt chart (Appendix 7). Given the very tight timeline after funding was provided to DMS (10 months), rigorous adherence to the timeline was necessary to ensure that all work was completed for the 86th Legislative session. The remainder of the report is the output of this approach and these processes.
Figure 1. Preplanning Structure for ASH Brain Health System Redesign
Key Points – Approach
• HHSC contracted with DMS to lead a redesign process for the ASH Campus and Service Area.• A wide range of stakeholders from the region actively contributed to plan development.
• Planning was guided by several principles, with improving the care of people being the first of those.