06. Epidemiologic Considerations
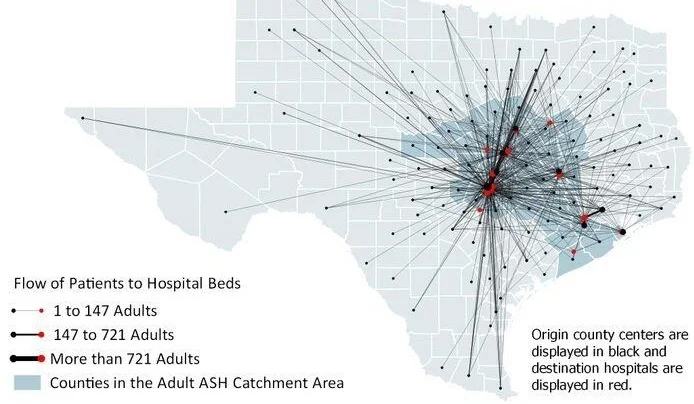
Meadows Mental Health Policy Institute generated epidemiological data including this map of County-to-Hospital Patient Flows (Adults). The 38 counties serving adults in the ASH service area are darkened.
Rates of mental health disorders are entirely predictable in even modest-sized populations, as they are minimally impacted by race or ethnicity, and they tend to occur similarly across states, nations and cultures. Consequently, the potential unmet need in the ASH Service Area can be estimated based upon known rates of psychiatric conditions compared against current levels of treatment. Tables 18 and 19 provide estimated prevalence of serious mental illness (SMI) and related conditions for the counties comprising the ASH Service Area. These data are also available at the county level in Appendix 12. To provide a sense of relative scale, we first report the population of these counties, then, because the state hospital disproportionately serves people living in poverty, we report the population living in households with incomes below 200% of the federal poverty level.
The LMHAs provide outpatient services to people who have a diagnosed serious mental illness; however, LMHAs are not sufficiently funded to meet 100% of the potential demand for services. As illustrated in Appendix 12, the ASH service area is consists of approximately 600,000 people who have a need for mental health services. Of the 20% of people in the service area who need services an average of only 7.5% of people actively seek and receive care at their local LMHA. The US Census Bureau estimates that approximately one half of people in the US have employer sponsored insurance that covers mental health services. Unfortunately, there is a shortage of mental health providers, especially psychiatrists, who will take insurance, so that most psychiatric clinics in the Service Area have waitlists themselves (see “Workforce” section of this report). According to Milliman (2018) we estimate 250,000 people, including those with and without private insurance, in the ASH Service Area are either not receiving care or are unable to adequately access care in their community.
“mental health disorders...are minimally impacted by race or ethnicity, and they tend to occur similarly across states, nations and cultures.”
Based on diagnosis and past use of the emergency department and inpatient services, about 2,000 adults at any time are estimated to have the most intensive needs. These individuals tend to cycle frequently between hospitals, emergency rooms, community placements and, too often, adverse conditions such as homelessness and contact with the judicial system. This level of illness severity equates with the most intensive level of community need in Texas, which qualifies the person for the evidence-based model of Assertive Community Treatment (ACT). Additionally, we estimate another 2,000 adults who are primarily cycling between the correctional system and the community, in addition to using elevated levels of inpatient, emergency room, and other services. These individuals would qualify for Forensic Assertive Community Treatment (FACT), which can reduce both inpatient bed use and criminal justice involvement. Current capacity to meet these high-service need groups within the Service Area (654 individuals) provides less than 50% of the demand.
“…about 2,000 adults at any time are estimated to have the most intensive needs.”
The most common diagnosis of adults and youth with serious mental illness is major depressive disorder that often is not addressed in public mental health program planning. The generally more severe disorders of bipolar, schizophrenia, and schizoaffective disorders, which are more common for patients at ASH and for people in the community in need of ACT and FACT services, are relatively less common in the ASH Service Area population. Major depression and the depressive phase of bipolar disorder are the most common conditions linked to suicide.
The future prevalence of these mental health conditions will be determined in part by early and effective community-based treatment, but largely by population growth in the counties served by the Austin State Hospital. Population projections are created by the Texas State Demographer for each county in Texas (TXPop). Table 19 summarizes adult population projections for the ASH Service Area. Projections to 2050, and for other age groups, are available at Appendix 12. Absent changes in other factors that influence mental health service needs, the growth in population will result in approximately the same increase in demand for services, including inpatient facility capacity.
Key Points – ASH Service Area: Epidemiological Considerations
• Nearly 600,000 individuals in the ASH Service Area are expected to need mental health services. The public mental health system only addresses a fraction of these needs.• The Central Texas population is rapidly growing, which will further stress existing mental health services.
• The growing need cannot be managed simply by adding more hospital beds.