04. Courts and Jails as Providers of Mental Health Care
The ASH Brain Health System Redesign team visited Steering Committee member Sheriff Dennis Wilson at the Limestone County Jail to observe and learn more about the mental health needs of rural communities, law enforcement, jails, and the people that they serve.
Managing Adults in Jails
Police and sheriff departments are often frontline managers of mental health crises within the ASH Service Area, as well as throughout the state and nation. Consequently, local and county jails must care for people with mental health conditions while processing legal charges. These charges frequently stem directly from behaviors involving the person’s mental illness or in the process of trying to getting them into care (e.g., pushing a police officer as she tries to wrestle the individual into a squad car to get them to an emergency room, producing an assault charge). Treatment Advocacy Center reports that state prisons hold more people with mental illnesses than hospitals; the ASH Service Area contains 46 state prison units, 4 private prisons, and 72 jails. The area also has 195 specialty courts and over 150 criminal courts, although only 7 mental health courts.
The jails in the ASH Service Area manage individuals with mental illness who are deemed incompetent to stand trial following procedures in Article 46B. This population includes individuals charged with both misdemeanors and felonies. Individuals charged with one of the 13 legislatively mandated offenses are placed in maximum-security psychiatric units for competency restoration; they do not come to ASH. In 2018, 322 individuals were admitted to ASH directly from criminal courts or jails under 46B processes. Additionally, as discussed previously in this report, approximately 75 people with mental illness await referrals from jails to ASH for inpatient competency restoration at any given time. In many circumstances, inadequate mental health support within the jails delays or creates discontinuity in the delivery of psychiatric care, so these same individuals are often not receiving adequate treatment. These impediments extend the episode of illness and suffering for the person with mental illness while also limiting the ability of legal personnel to provide assistance and process criminal charges.
Juvenile Detention Centers and Juvenile Justice Courts
Juvenile detention centers and justice courts generally serve youth, ages 10–17 years old. All youth who enter a juvenile detention facility for short-term probation or longer-term residency are screened for mental health conditions using the Child and Adolescent Needs and Strengths (CANS) tool. The Hogg Foundation for Mental Health estimates that 70% of youth in the juvenile justice system have mental health conditions; this percentage is over three times larger than the 20% of youth with mental health conditions in the general population. Of note, Travis County offers the Collaborative Opportunities for Positive Experiences (COPE), a juvenile justice deferred prosecution program that serves youth from age 10 - 17 who have a mental health diagnosis that has contributed to the commission of a juvenile offense. COPE diverts young offenders from court proceedings and criminal involvement by providing mental health services, community linkage and treatment for the juvenile and family through community collaborations.
While in pre- or post-adjudication residency at a Texas Juvenile Justice Department (TJJD) facility, youth receive their mental health services through TJJD. In 2015, the Legislative Budget Board (LBB) estimated that each youth in a residential facility costs, on average, $437 per day. This cost far exceeds average daily costs for youth on parole ($32 per day) or youth on probation ($5 per day). It also exceeds standard intensive outpatient care ($75 per day). For FY16 and FY17, the Texas Legislature appropriated approximately $85 million to TJJD for behavioral health purposes; this funding stream is entirely separate from funds managed by HHSC for other parts of the care continuum, complicating referrals. Occasionally, a youth may be transferred to ASH Child and Adolescent Program Services (CAPS) for court-mandated medication administration if it cannot be delivered in the detention center (although this referral occurs rarely).
“…70% of youth in the juvenile justice system have mental health conditions…”
For both adults and youth, there are also significant costs associated with the transportation and detention in the justice system of individuals with mental illnesses, as illustrated in Table 13 that is updated from a prior report by the Meadows Mental Health Policy Institute (MMHPI (2015)). A better-integrated system could shift some of these expenses toward alternative, more effective uses. We discuss in the “Statement of Needs and Recommendations” section of this report the potential impact on waitlists if bed turnover at ASH is accelerated.
Competency Restoration
Texas Code of Criminal Procedures Article 46B defines a person as incompetent (1) if he or she does not have sufficient ability to consult with an attorney with reasonable and rational understanding or (2) if the person does not have a rational and reasonable understanding of the proceedings against him or her. “Competency restoration” refers to the educational process of assisting people with mental illness who are facing legal charges to participate in their own defense by enabling them to understand the court process and the charges against them. It is typically assumed that competency restoration is synonymous with symptom improvement; in fact, although somewhat associated, they are relatively independent processes. Many patients with even marked symptoms are still able to understand and participate in legal proceedings and paradoxically, some with less severe or few symptoms are not. Clinical improvement is a medical process whereas competency restoration is an educational process.
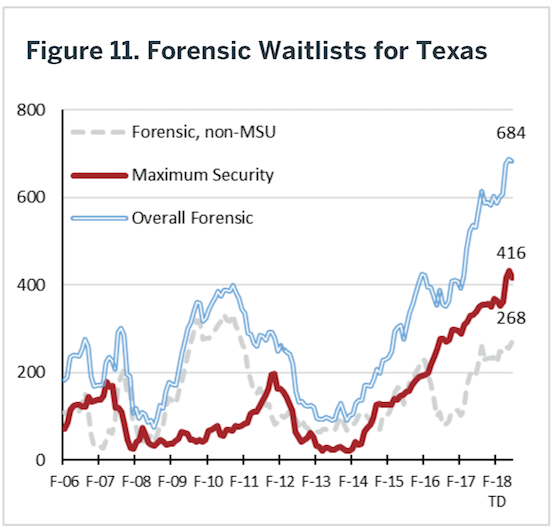
Under Article 46B.071(a), Texas Code of Criminal Procedure, when a defendant is found to be incompetent to stand trial, the court will (1) release the defendant on bail and order the defendant to participate in an outpatient competency restoration program or (2) commit the defendant to a state hospital or a jail-based competency restoration program for competency restoration services. In the absence of sufficient outpatient and jail-based competency restoration programs, inpatient hospitalization is the default even when not necessary from a clinical perspective. In fact, hospitalizing an individual for competency restoration when clinically they could be treated in an alternative venue violates their rights to receive psychiatric treatment in the least restrictive environment. Because state hospitals, in particular, lack adequate space and resources, defendants are then placed on waitlists until a forensic bed becomes available as noted. Long waits in jail waiting for hospital admission appears to violate an individual’s right to a speedy trial. Figure 11 illustrates the growth in Texas generally in these waitlists over the past several years.
“Clinical improvement is a medical process whereas competency restoration is an educational process.”
Determining competency for a child or youth defendant differs from that for adults, in both the language and sought outcome of the initial evaluation. Texas Family Code Title 3 Chapter 55 defines a child or youth in juvenile court as unfit to proceed if he or she, due to a serious mental illness or intellectual disability, lacks capacity to understand the proceedings in a juvenile court or to assist in his or her own defense. Furthermore, the child or youth shall not be subjected to discretionary transfer to criminal court, adjudication, disposition, or modification of disposition as long as incapacity endures.
Historically, competency restoration was not permitted outside of an inpatient setting. However, Texas law now permits competency restoration in jail and in community settings. Texas currently has 12 outpatient competency restoration programs administered by the LMHAs. The Austin State Hospital Service Area has four such programs to accommodate the growing need of the forensic population. The first program began in 2008, two programs were added in 2012, and the fourth program began in 2013. However, despite the emergence of these programs, waitlists for competency restoration services continue to be lengthy. According to the Meadows Mental Health Policy Institute, data from June 2018 showed that of the 792 individuals on waiting lists for state hospitals, the vast majority was waiting for forensic beds. These include 428 people on the maximum-security unit (MSU) waiting list, with an average wait of 164 days (ASH does not contain an MSU). Another 258 people were on the forensic non-MSU waiting list, with an average wait of 31 days. People on these forensic waitlists may be housed in jail for weeks or months without receiving proper mental health treatment.
“…Texas law now permits competency restoration in jail and in community settings.”
Then, once admitted to a state hospital bed, the competency restoration process adds dramatically to the length of stay – on average, 105 days in the Austin State Hospital. In contrast, in urban centers, lengths of stay to stabilize psychiatric symptoms typically average below six days. As noted in the discussion of ASH performance, in general, competency restoration can be completed within 60 days (and typically in less than 3 weeks (Gillis et al., 2016)).
State law requires that people found incompetent and charged with one of 13 specific crimes (e.g., murder, kidnapping, indecency with a child) must be confined in a maximum-security unit (MSU). When a bed opens at an MSU, the person will be transferred from the county jail to the MSU. Once the individual arrives at the MSU, the Dangerousness Review Board must conduct a hearing; however, that process takes significant time. The requirement that people must be committed to the MSU based solely on their charge (rather than clinical condition), combined with lengthy delays in accessing a bed, adds to the jail waitlists, intensifying stress on local jails and their staff, as well as the individual waiting for a hospital bed to become available. Re-evaluating whether some of these individuals could be managed outside MSUs might assist these waitlists; however, even if this decision was made today, non-MSU options are also not available until ASH (and other state hospitals) capacity is increased.
Competency Restoration Costs
Inpatient competency restoration is expensive. As described in Table 14 for a ‘typical’ individual, the total expense exceeds $75,000. Some of these costs are driven by maintaining individuals in higher levels of care (e.g. hospitalization) than clinically indicated due to legal rather than clinical discharge decisions. Inpatient competency restoration is the current default approach in the ASH Service Area, although alternative pathways that are used both in Texas and other states provide less expensive and more clinically effective alternatives. In the waitlist period in jail, clinical care may be delayed. Table 15 provides an alternative pathway based on an intensive outpatient (IOP) competency restoration with a concurrent embedded FACT (Forensic Assertive Community Treatment) team. We stretched the duration of the calculation to be equivalent to the inpatient example, even though it likely would be shorter and transition to even less expensive standard outpatient care. In this case, the individual would have to be determined safe in the community for himself and others, but then otherwise could proceed through the competency restoration process to allow legal charges to be adjudicated or dismissed as with any other defendant. As noted in Table 15, the cost of this approach is almost five times less expensive than the default ASH inpatient approach and clinical care begins immediately. The ASH Service Area has, unfortunately, limited FACT programs (32% of the LMHAS, see “Outpatient Service Utilization” section of this report). As a second alternative example, Table 16 portrays use of a private-hospital purchased rapid-stabilization inpatient stay prior to essentially the same pathway illustrated in Table 15. Even with this inpatient component, the overall approach is 2/3 less expensive than the state-hospital-based approach, and again care begins immediately. A number of other alternative models can be developed in which individuals receive care more quickly at less cost. These approaches could save millions of dollars in the ASH Service Area. For example, if only half of the 386 individuals who underwent competency restoration during a typical recent year were evenly alternatively managed between these other two pathways, more than $10M would have been saved. References for Tables 14 – 16 can be found in Appendix 14.
Currently, there is a conflation between legal and clinical pathways in people undergoing competency restoration to prepare to stand trial. Ultimately, separating these processes to permit clinical care to occur in the least restrictive, most appropriate setting possible while concurrently providing the educational processes for competency restoration suggests these processes should be separated. Namely, statute changes as necessary to permit wider use of alternative pathways that assign clinical design making within healthcare systems and legal designs (e.g. competency) within legal systems would improve both clinical and legal outcomes while ultimately reducing costs. Recommendations to that end are discussed in the “Statements of Need and Recommendations” section of this report.
Involuntary Civil Commitment
In addition to the competency restoration component of the legal process, Texas law provides an evaluation and treatment alternative referred to as “Involuntary Civil Commitment.” This civil procedure is a last resort for people who are not able to care for themselves or are at imminent risk of harm to themselves or others. In Texas, the civil commitment process is initiated by a peace officer who believes that (1) a person has a mental illness; (2) because of the mental illness, the person poses a serious risk to self or others unless immediately restrained; and (3) there is insufficient time to obtain a warrant. The person is transported to the nearest inpatient facility or a mental health facility that the Local Mental Health Authority believes is appropriate in the absence of an inpatient facility. In addition to initiating the process by a peace officer, Texas law also provides that an individual can petition a court to issue a warrant for the person’s detention based on the applicant’s belief that the person is a risk to self or others and providing specific evidence of behavior, threats, acts, or attempts illustrating risk. If the court issues a warrant, the person is transferred by a police officer to a facility.
Once detained, the person can be held for observation for up to 48 hours (or if a weekend or holiday intervenes, through 4:00 p.m. of the following business day). The person must be examined by a physician within 12 hours, and the physician must certify to the facility that the person has a mental illness and is a risk to self or others, providing evidence in support of that opinion. A person detained for observation is entitled to a probable cause hearing within 72 hours of the initial detention. The evaluation results are then presented to the probate court/magistrate in the form of a medical certification recommending further confinement. The court may grant an Order of Protective Custody to extend the person’s confinement pending further hearings on extended commitment. For the person to be held further, a final hearing must be set within 14 days of the initial application and be held within 30 days of that filing. This more formal hearing requires at least two medical certificates. The person may be ordered into treatment, not to exceed 90 days, at the end of the hearing.
Finally, the law permits the court to order extended mental health services after a hearing. However, this order can only be entered for someone who has received court-ordered inpatient services under a civil or criminal court order for at least 60 days in the prior 12 months or 60 days of court-ordered outpatient services during the preceding 60 days. Extended treatment can be ordered for no longer than 12 months. In each of these situations, commitment requires a finding that the person has a mental illness. In addition to this finding, there must be evidence of a recent act or continuing pattern of behavior that “tends to confirm” the likelihood of serious harm to self or others or that causes the person to be unable to meet basic needs such that commitment is necessary.
In addition to waitlists for admission for competency restoration, there are waitlists for people awaiting civil admission to a state hospital, although these tend to be quite a bit smaller (typically about 20 people per day). Additionally, some individuals in competency restoration may be better served by dropping charges and transferring into the civil commitment process. Alternative pathways through the intersection between the legal and mental health care systems could significantly improve effectiveness and efficiencies of both sets of processes.
Key Points – ASH Service Area: Courts and Jails
• Waitlists in jails delay both treatment and timely resolution of legal charges for Texas residents.• Competency restoration procedures are overly complex and conflate clinical need for treatment with inability to participate in legal decision making.
• There are limited competency restoration programs outside ASH in the Service Area, even though statutes now support these alternatives.
• Alternative competency restoration pathways could provide better clinical and legal outcomes at a substantially reduced cost.